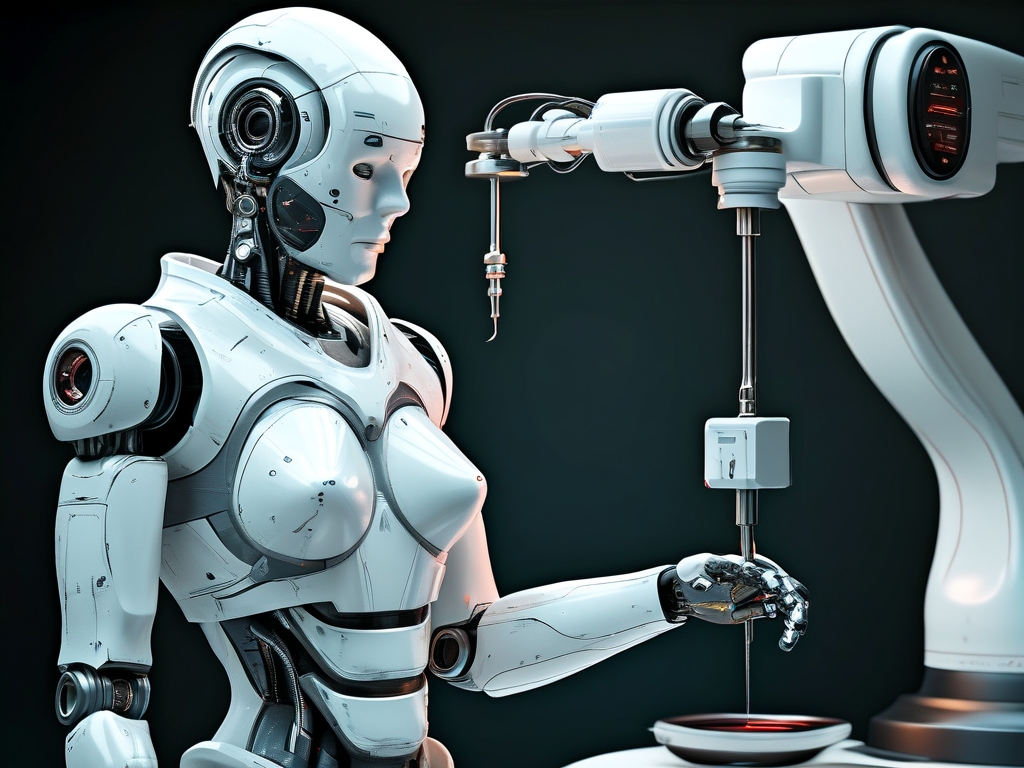
The integration of robotics into medical procedures has revolutionized healthcare, and one of the most groundbreaking advancements is robotic needle insertion technology. This innovation combines precision engineering, artificial intelligence (AI), and real-time imaging to enhance the accuracy of minimally invasive procedures. From biopsies to drug delivery, (robotic needle insertion technology) is reshaping diagnostics and treatment protocols across multiple medical disciplines.
The Mechanics of Robotic Needle Insertion
At its core, robotic needle insertion systems rely on three key components:
- Advanced Imaging Integration: High-resolution ultrasound, MRI, or CT scans provide real-time anatomical data, enabling the robot to map insertion paths with submillimeter accuracy.
- AI-Driven Path Planning: Machine learning algorithms analyze patient-specific data to predict tissue resistance, avoid critical structures like blood vessels or nerves, and adjust trajectories dynamically.
- Haptic Feedback Mechanisms: Force sensors and actuators mimic the tactile sensitivity of human hands, allowing surgeons to maintain control while reducing hand tremors.
Clinical Applications
-
Cancer Diagnosis and Treatment
- Biopsies: Traditional manual biopsies often require multiple attempts to capture viable tissue samples, increasing patient discomfort and risk. Robotic systems, such as the FDA-approved "Artemis," achieve 98% accuracy in targeting tumors, even in hard-to-reach areas like the prostate or pancreas.
- Radiofrequency Ablation: In liver cancer treatment, robots precisely guide needles to deliver thermal energy, destroying tumors while sparing healthy tissue. Studies show a 30% reduction in collateral damage compared to manual methods.
-
Pain Management and Anesthesia
- Epidural Injections: Robotic systems like "Epione" enhance the success rate of epidural needle placement from 70% (manual) to 95%, critical for obstetric patients during childbirth.
- Nerve Blocks: For chronic pain sufferers, robots use 3D mapping to administer localized anesthesia with minimal risk of nerve injury.
-
Neurological Interventions
- Deep Brain Stimulation (DBS): Parkinson’s patients benefit from robotic insertion of electrodes into specific brain regions, improving surgical outcomes by 40%.
- Intrathecal Drug Delivery: Robots enable precise catheter placement for administering chemotherapy or painkillers directly into the spinal fluid.
Advantages Over Traditional Methods
- Precision: Human hands inherently face limitations due to tremors (averaging 50–100 microns). Robots reduce positional errors to under 10 microns.
- Reduced Complications: A 2023 meta-analysis in The Lancet found robotic needle procedures lowered infection rates by 22% and shortened recovery times by 35%.
- Accessibility: Teleoperated systems allow specialists to guide procedures remotely, bridging gaps in rural healthcare.
Challenges and Ethical Considerations
Despite its promise, the technology faces hurdles:
- Cost: Initial setup costs exceed $500,000, limiting adoption in low-resource settings.
- Training: Surgeons must master hybrid skills, blending traditional expertise with robotic interface navigation.
- Ethics: Overreliance on automation risks deskilling healthcare providers, raising debates about responsibility in case of malfunctions.
Future Directions
- Nanoscale Robotics: Researchers are developing microneedles equipped with sensors to monitor biochemical changes in real time.
- Autonomous Systems: AI models trained on millions of procedural datasets may one day perform unsupervised insertions in emergency scenarios.
- Biodegradable Needles: MIT’s 2024 prototype dissolves after drug delivery, eliminating removal procedures.
Robotic needle insertion technology represents a paradigm shift in minimally invasive medicine. By merging human expertise with machine precision, it addresses longstanding challenges in accuracy, safety, and accessibility. As costs decline and AI evolves, this technology will likely become standard practice, transforming everything from routine blood draws to life-saving cancer therapies. The future of healthcare isn’t just automated—it’s intelligently adaptive.