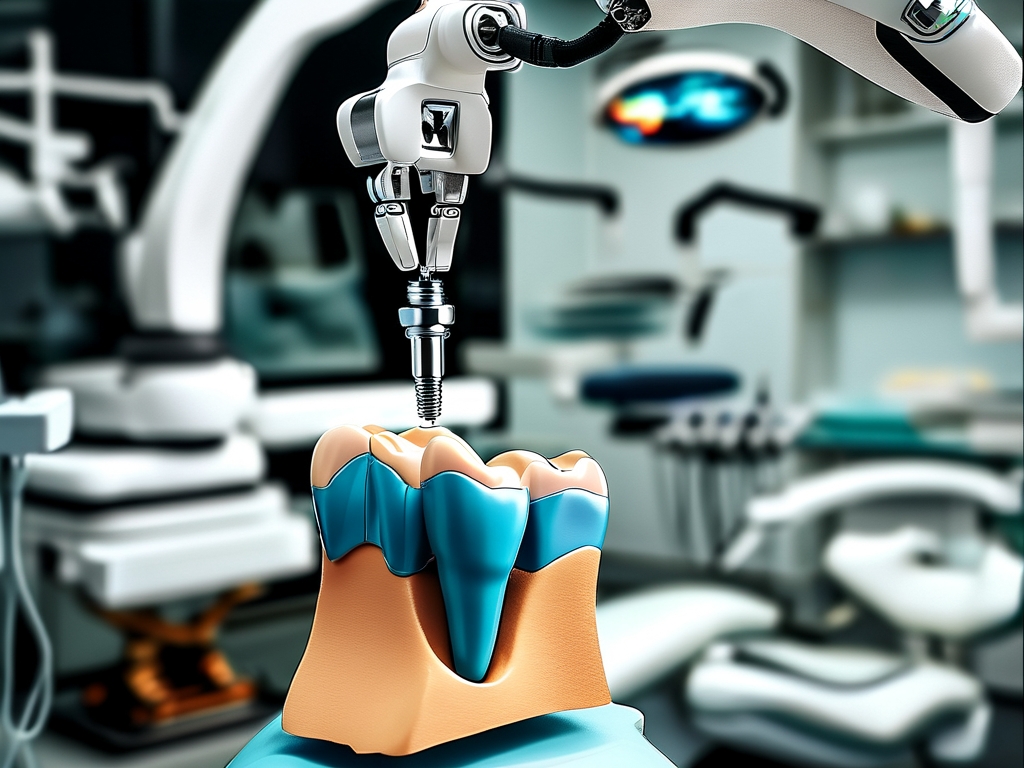
The integration of robotics into dental implantology has revolutionized oral surgery, offering unprecedented accuracy and predictability. At its core, robotic dental implant technology combines advanced imaging, artificial intelligence (AI), and precision mechanics to optimize every stage of the procedure—from preoperative planning to postoperative recovery. This article explores the scientific principles behind this groundbreaking innovation and its transformative impact on patient care.
Foundation of Robotic Implant Systems
Robotic systems for dental implants rely on three interconnected components: 3D imaging, dynamic navigation, and automated surgical tools. High-resolution cone-beam computed tomography (CBCT) scans generate detailed models of a patient’s jawbone, soft tissues, and nerve pathways. These datasets are processed by AI algorithms to create a customized surgical blueprint, accounting for bone density, anatomical constraints, and ideal implant positioning. Unlike traditional freehand methods, robotic arms execute the plan with submillimeter precision, minimizing human error.
A key innovation is real-time feedback adaptation. During surgery, optical tracking cameras monitor the patient’s head movements and adjust the robotic arm’s trajectory instantaneously. This ensures the drill maintains alignment with the preplanned path even if the patient shifts slightly—a critical feature for avoiding sensitive structures like the inferior alveolar nerve.
Workflow: From Digital Design to Physical Execution
- Virtual Planning: Surgeons use specialized software to simulate implant placement, testing multiple angles and depths virtually. This step reduces chair time and allows patients to visualize outcomes beforehand.
- Guided Osteotomy: The robotic arm prepares the implant site using calibrated drilling sequences. Force sensors detect variations in bone density, automatically adjusting speed and pressure to prevent overheating or microfractures.
- Prosthetic Integration: Post-placement, digital impressions are taken to design crowns or bridges that fit seamlessly with adjacent teeth. Some systems even enable same-day restorations using in-office milling machines.
Clinical Advantages Over Conventional Methods
Studies show robotic-assisted implants achieve 98.5% accuracy in positioning compared to 85–90% with manual techniques. This precision translates to fewer complications, such as peri-implantitis or nerve damage. Additionally, flapless surgeries—where gums remain unopened—are more feasible with robotics, cutting recovery time by up to 40%. Patients also benefit from smaller incisions, reduced swelling, and lower infection risks.
Economically, while initial costs are higher, robotic systems reduce long-term expenses by minimizing revision surgeries and enhancing implant longevity. Practices adopting this technology report higher patient satisfaction rates due to predictable outcomes and minimally invasive experiences.
Challenges and Future Directions
Current limitations include the learning curve for clinicians and the need for standardized protocols. However, next-gen systems aim to integrate augmented reality (AR) for enhanced visual guidance and machine learning to refine planning algorithms based on global case databases. Researchers are also exploring biodegradable robotic tools for temporary bone stabilization during healing.
In , robotic dental implant technology represents a paradigm shift in oral rehabilitation. By merging engineering rigor with clinical expertise, it sets new benchmarks for safety, efficiency, and patient-centered care—ushering in an era where perfect smiles are engineered, one algorithm at a time.