In the rapidly evolving landscape of healthcare, robot-assisted disease diagnosis technology has emerged as a groundbreaking innovation, promising to transform how medical professionals detect and treat illnesses. By integrating artificial intelligence (AI), machine learning, and advanced robotics, this technology enhances diagnostic accuracy, reduces human error, and streamlines patient care. This article explores the mechanisms, applications, benefits, and ethical considerations of robotic disease diagnosis systems, shedding light on their potential to redefine modern medicine.

The Mechanics of Robotic Diagnosis
At its core, robotic disease diagnosis relies on AI algorithms trained on vast datasets of medical records, imaging scans, and biochemical markers. These systems analyze patient data-such as X-rays, MRIs, blood tests, or genetic profiles-to identify patterns indicative of specific conditions. For instance, AI-powered robots can detect early-stage tumors in radiology images with precision surpassing human radiologists in some cases. Machine learning models continuously improve by incorporating new data, enabling robots to adapt to emerging diseases or rare disorders.
Robotic hardware complements this software-driven analysis. Surgical robots, like the da Vinci Surgical System, already assist in minimally invasive procedures, but diagnostic robots take automation further. Portable devices equipped with sensors can perform real-time monitoring of vital signs, while larger systems automate laboratory processes, such as sequencing DNA or processing biopsies. These technologies minimize delays in diagnosis, critical for time-sensitive conditions like sepsis or heart attacks.
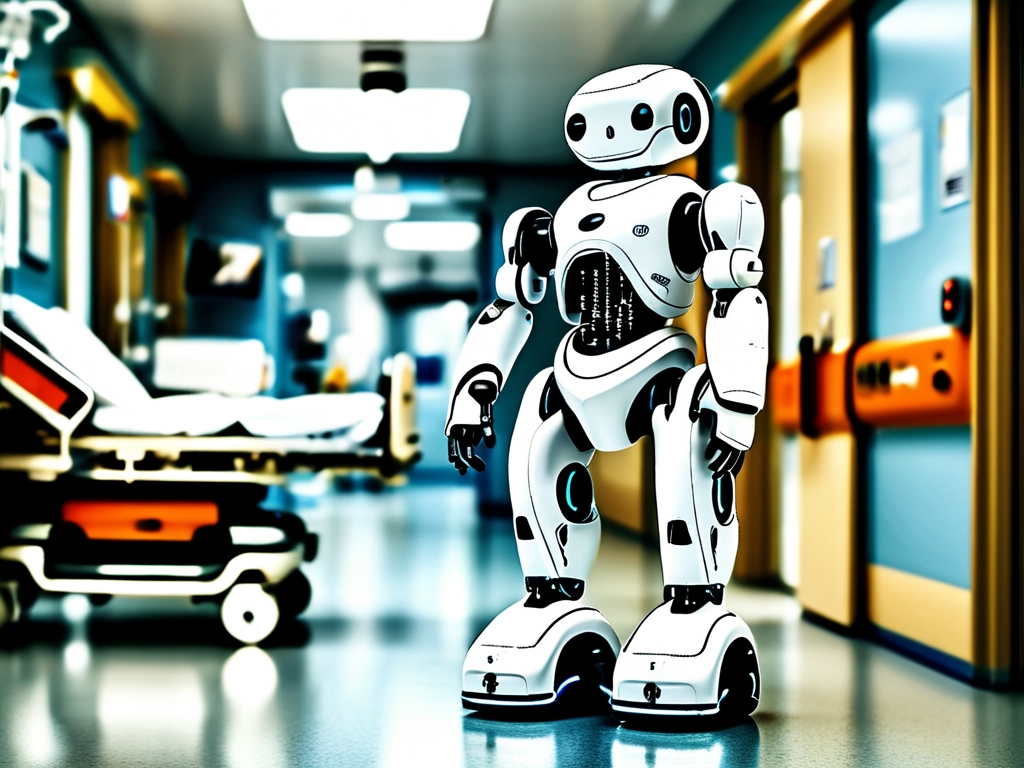
Applications Across Medical Fields
Robotic diagnosis is revolutionizing multiple specialties. In oncology, AI systems like IBM Watson for Oncology analyze patient histories and research databases to recommend personalized treatment plans. In cardiology, wearable robots track heart rhythms and predict arrhythmias before symptoms manifest. During the COVID-19 pandemic, robots were deployed to analyze throat swabs and CT scans, reducing exposure risks for healthcare workers.
Mental health is another frontier. Chatbots like Woebot use natural language processing to screen for depression or anxiety, offering preliminary assessments and coping strategies. While not replacements for human therapists, they bridge gaps in access to care, particularly in underserved regions.
Advantages Over Traditional Methods
The benefits of robotic diagnosis are multifaceted. Speed is a key advantage: AI can process terabytes of data in seconds, whereas humans might take days. Accuracy also improves; studies show AI reduces misdiagnosis rates by up to 40% in fields like dermatology and ophthalmology. Additionally, robots operate without fatigue, eliminating variability caused by human stress or burnout.
Cost-effectiveness is another advantage. Automated systems lower long-term healthcare expenses by catching diseases early, reducing hospitalizations. For example, diabetic retinopathy screenings conducted by AI in rural India cut costs by 80% compared to traditional methods.
Ethical and Practical Challenges
Despite its promise, robotic diagnosis faces hurdles. Data privacy is a major concern: sensitive patient information must be protected from breaches, especially when stored in cloud-based systems. Bias in AI models is another issue; if training data lacks diversity, robots may underperform for certain demographics. For instance, skin cancer algorithms trained predominantly on lighter skin tones have shown reduced accuracy for darker-skinned patients.
Regulatory frameworks lag behind technological advancements. Governments struggle to standardize validation processes for AI diagnostics, raising questions about liability in case of errors. Moreover, over-reliance on robots risks dehumanizing healthcare. Patients may distrust machines delivering life-altering diagnoses, preferring empathetic human interaction.
The Future of Robotic Diagnosis
The trajectory of this technology points toward greater integration. Future systems may combine diagnosis with treatment, such as nanobots that detect and destroy cancer cells autonomously. Collaboration between robots and humans will likely define next-generation care: AI handles data analysis, while doctors focus on complex decision-making and patient communication.
Global adoption hinges on addressing disparities. While wealthy nations pioneer these technologies, low-income regions need infrastructure investments to benefit. Initiatives like the WHO's AI for Health program aim to democratize access, ensuring equitable distribution of robotic diagnostic tools.
Robot-assisted disease diagnosis represents a paradigm shift in medicine, blending cutting-edge technology with clinical expertise. While challenges remain, the potential to save lives, reduce costs, and improve healthcare accessibility is immense. As society navigates ethical dilemmas and refines these systems, one truth becomes clear: the future of diagnosis is not human versus machine-it is human and machine, working in harmony.